Last week, I talked about just what stress actually is. This week, you're going to learn about what stress does to our muscles, tendons, joints, and nerves. I'll list the three most common painful conditions that are caused by stress and provide some information on what you can do about it if you're suffering with those conditions.
First, there's a little bit of background you need to have. Many of us have probably heard about our fight, flight, freeze system. Our nervous system is broken down into three categories.
The autonomic nervous system is the part that is most affected by stress. This system is broken down into two parts, the sympathetic nervous system and the parasympathetic nervous system.
The sympathetic nervous system is what is normally referred to as our fight or flight system and the parasympathetic nervous system is often referred to as the rest and digest system.
The sympathetic and parasympathetic systems are both always online in your body. However, if you're walking through the woods and a bear jumps out and starts chasing you, your parasympathetic nervous system will dial way down in function, and your sympathetic nervous system will turn way up. The sympathetic nervous system is meant to protect us from danger. However that system is meant to only be on full blast for short periods of time.

Normally, if that bear jumps out in the woods, the sympathetic nervous system shoots up to overdrive, pumps more blood to your muscles so you can run faster, and usually within 5 to 10 minutes - it's over, one way or the other. You either got away from the bear or you didn't, but either way, the system then is meant to go back to normal.
But we sit in traffic stressed to the max for hours at a time.
And during that time our sympathetic nervous system is running continuously.
That's where the problems occur.
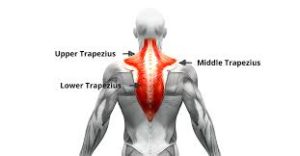
Our bodies can function pretty well with increased activation to those muscles for a short period of time. But if it continues day after day in our stressful lives, then it starts to cause problems. It starts to cause pain and tension on both sides of the neck, it can cause shoulder problems due to the fact that this raises the shoulder from its normal resting position and makes it more vulnerable, and it can cause pain in between the shoulder blades from the tension of all those muscles.
2. The second most common musculoskeletal consequence of increased stress is pain in the jaw. It is very common that when people are under stress, they will clench their jaw as a compensatory strategy. This constant tension can create pain in the muscles surrounding the jaw as well as pain in the jaw joint itself.
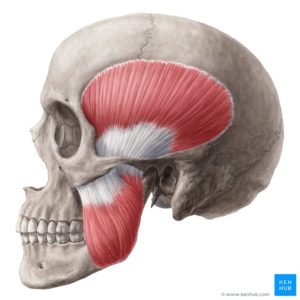
But clenching the jaw is not only a problem for the jaw itself. The way that the muscles in our head and neck work, when you clench your jaw, you clench your neck. So not only does teeth/jaw clenching lead to pain in the jaw, but it can also lead to neck pain as well as headaches. The type of headaches that it causes are referred to as tension headaches. These headaches are felt at the base of your skull and around the sides of your head.

3. The third most common musculoskeletal issue caused by stress is low back pain. The jaw is not the only area that people clench when they are stressed. There are two other areas that are very common for people to clench during times of stress. These are the abdominal muscles and the gluteal muscles.

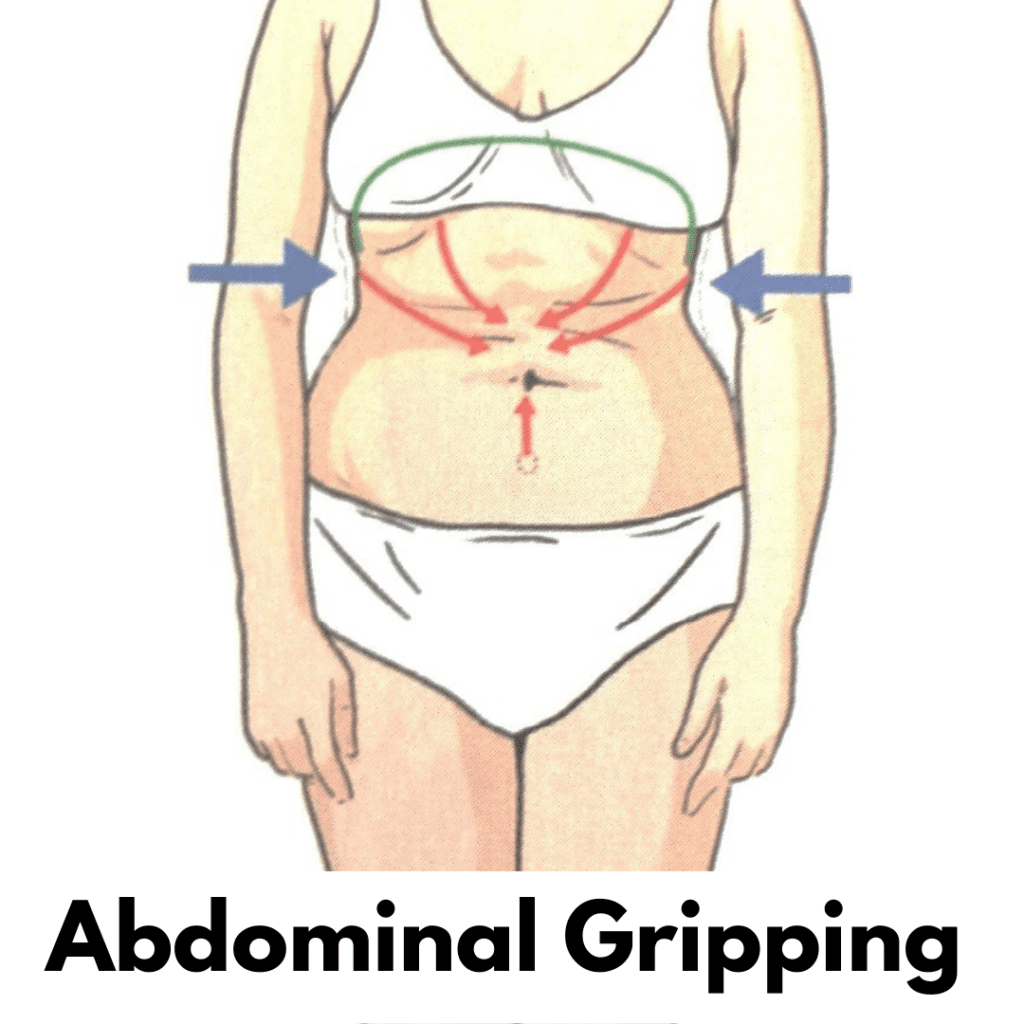
Excessive clenching in either of those two areas is known to lead to low back pain. There is a phenomenon in the body called irradiation. This phenomenon basically means that tension breeds tension. An example of this is if you were trying to lift something heavy with your right arm, and it was difficult, you might clench your left fist really tightly in order to build more strength in your right arm. So basically, creating tension in a nearby area increases the tension in that secondary area.
Increased tension in the abdominal muscles leads to increased tension in the low back muscles which will lead to pain. The same thing happens in the gluteal muscles. Our muscles are meant to work all together. When one group becomes dominant and overactive, this causes tension to increase all around that area.
If you're reading this and you are thinking that you can really relate to those three areas that I talked about above, you're probably wondering, "Well, what can I do about it.?"
There are two main things that need to be done for these problems to improve. The first is: you need to develop strategies for managing stress.
None of us can avoid stress. It's just a part of life. However, that doesn't mean that we just say woe is me and do nothing. So that means, if certain times of our life become more stressful than normal, we'll want to find strategies to mitigate the stress. I will talk about some specially helpful strategies in further blogs.
In conjunction with managing your stress, you want to find ways to alleviate the tension in the areas that are bothering you. Below, I will go over great ways to reduce the tension in the three areas I talked about above.
The contract-relax stretch is shown below. This type of stretch involves activating the muscle first and then stretching it. After a muscle has been activated, it's actually more susceptible to stretch.
2. For the inner shoulder blade muscles, I recommend using a lacrosse ball or trigger point ball.
a) For this, you're just going to go stand with your back against a wall. b) Put a lacrosse ball in between your shoulder blade and your spine. c) Then you're just going to move your torso and bend your knees in order to roll the ball all the way into the muscles in between the shoulder blades.
I recommend 60 to 90 seconds on each side of the spine.
For the jaw muscles, there are two main areas that need to be worked on. These are the jaw muscles, and the upper neck muscles. As I said before, clenching can cause both jaw pain and headaches that tend to be at the base of the skull.
a) The first technique is a release of the tension in your jaw muscles. For this one you're going to take your fingers and find your cheekbones and follow your cheekbones back towards your ear. There are two main groups of job muscles that we want to release. One of them is above the cheekbones and the other one is below.
b) So first, we'll start on the ones above the cheekbones and you'll just move your fingers upwards into the area just in front of your ear. You're going to push your hands inwards like you're trying to go into your skull and then kind of drag the tissue up towards the ceiling. This pins the muscle. Then you're going to slowly open your jaw as wide as you can: this will stretch the muscle. The video below shows the release for the muscle that is above your cheekbones. You would just repeat the same technique in the muscles below your cheekbones.
The image below shows the locations of these muscles so you'll want to do multiple passes with your hands since the muscles are pretty large.
3. The last area are the muscles at the base of your skull. These are the muscles most commonly affected when we clench our teeth. And these are the muscles most commonly associated with tension type headaches.
a) To work on these muscles, you're going to want to get either two tennis balls or two lacrosse balls and you're going to tape them together like the photo below. We call this device a peanut. b) What you want to do is to find a semi-hard surface and lie down on your back. c) Take the peanut and place it just below the base of the skull. d) You don't want the balls actually pushing on the bone of the skull - you want them in the fleshy area just below.
I recommend starting off by lying on this for 4 minutes at a time. Every couple of days, increase that by a minute until you get to 8 minutes. I don't recommend lying on it for longer than 8 minutes.
For the tightness that comes from gluteal muscle tension, we want to stretch out our hip muscles. The video below shows one of the best stretches to relieve tension in these areas.
If you are an abdominal gripper and notice tension in your abs daily ,the technique shown in the video below can be extremely helpful. He uses a much larger ball, but I recommend using a lacrosse ball in the same fashion as he shows in the video.
So there you have it. That darn stress really takes a toll on our body! But now you have some tools to fight back. Try these out and stay tuned for next week when I'll talk about stress management strategies.
And if you're dealing with a lot of pain right now and don't have time to wait for some of this stuff to work on your own, be sure to give us a call at 918-300-4084 and we can help you speed up that process of getting out of pain!


We have all heard that modern life is stressful. News articles talk about stress management, the health consequences of stress, and how to cope with stress. But ... what exactly IS stress?
With the holidays upon us, I wanted to do a deep dive on stress. During the month of December, I'm going to talk about the effects stress has on our bodies, and how to manage the stress we're all under.
In this first blog I'm going to talk about what stress is, what are the different types of stress, and what's the difference between stress and anxiety.
So what exactly is stress?
Stress is any type of change that causes physical, emotional, or psychological strain. Basically stress is your body's response to anything that requires attention or action.
But stress is not always a bad thing. There's actually two different types of stress: distress and eustress.

Distress is any stress that has a negative effect on us. It has the following characteristics:

Eustress is any stress that has a positive effect on us. The characteristics of eustress are:
Examples of distress would be things like the death of a loved one, losing your job, or experiencing a significant injury.
Examples of eustress would be things like getting a promotion at work, graduating from school, or winning the lottery.
One important thing to understand is that while both distress and eustress have very different effects on our mental and emotional health, they can both have detrimental effects on our bodies. They both can tax our body's reserves and produce negative physical effects. Stay tuned throughout this month and I'll go over many of the different negative physical effects of stress and what to do about them.
When you hear people talk about stress, it's common to hear them talk about anxiety as well. Those two terms are often presented as if they are the same thing. Stress and anxiety are definitely similar, but they are not the same thing.
What differentiates stress and anxiety is the source of the strain. The source of STRESS is external. This means the strain on the body is from outside. A work deadline, financial obligations, losing a loved one, these are all external factors. If the source of the strain is taken away, the strain goes away. If you complete that work project, the stress of the deadline goes away. If you come into some money, the stress of bills goes away. That is how stress works.
However, with ANXIETY, the source of the strain is internal. You can think of anxiety as what happens inside of us in response to stress. Maybe you start to worry constantly about money when you experience some financial difficulties, or perhaps a loved one dies and you start to become obsessed with the fear of your own death. These are both an internal response to stressors.
The main difference between anxiety and stress is that anxiety can remain long after the actual stressor has passed.
So there you have it. Now you know that there are actually two different types of stress. While their effects can be different, it's important to understand that they both drain the body's resources - so they can have negative effects. You also now know the difference between stress and anxiety. Mainly that stress is an external event and anxiety is how we deal with stress internally.
Stay tuned this month as I will be explaining the effects of stress on the body (You won't believe all the different ways it affects you!), and how to manage stress to reduce its harmful effects.
You are going to learn so much this month! Thanks for taking time out to educate yourself on stress/anxiety and how you can make your own life better by managing them.
Remember, this month often brings various external pressures to bear - and causes stress for a lot of us. We're here for you - we can help balance your body and alleviate some of the effects of that stress. We'd love to see you in our new location! Just give us a call at 918-300-4084

Last week I talked about how trigger points in our muscles can cause pain in other areas of the body and how this can trick us. However, muscle trigger points are not the only structures in the body that are known to cause referred pain.
Our internal organs can do the same thing. The most classic example of this is the heart. We all know that chest pain and left arm pain are signs of a heart attack. When the heart is irritated or under stress, it refers pain down the arm. This is a great example of why it's so important to see a doctor who understands referred pain.
Imagine going to the hospital with chest and left arm pain, and the doctor starts treating your left arm. If that happened to you, you're probably not going to have a very good outcome! Even though the pain is in the left arm, the only way to get the pain to go away is to treat the heart which is the source of the pain.
In this blog, I'm going to go over the three most common internal-organ referred pains that I see in patients at my clinic.
The number one most common internal-organ referred pain that I see is for kidneys. This pain referral pattern is most often seen during the formation of a kidney stone, but other problems with the kidneys can cause the same thing.
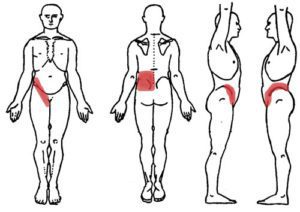
As you can see in the picture above, the kidney can cause pain in the lower back, in the outer hips, and in the front of the hips. The most common presentation is in the low back and specifically the sides of the low back. This is called flank pain.
If you are experiencing pain in these areas, there are a couple of ways to distinguish whether this is just normal back pain or if it might be coming from your kidneys. In regular low back pain, the source of the pain is usually in the muscles, ligaments, and joints of the spine.
Because of the tissues that are irritated in normal low back pain, the pain will normally fluctuate throughout the day, depending on the position of your body and your activities. So the pain might be better at certain times of the days, but get worse when you do certain activities because those tissues are being stressed.
When the pain is coming as referred pain from the kidneys, the pain is usually constant and doesn't change, no matter what you do. If you're having pain like this that is constant, your best bet is to see your primary care doctor instead of a chiropractor or physical therapist.
The second most common internal-organ pain referral that I see in my clinic is the gall bladder. This one can confuse a lot of people. The gall bladder refers pain to lots of different areas of the body and many times in the beginning stages, there's not a lot of hints that the gall bladder is actually having problems.
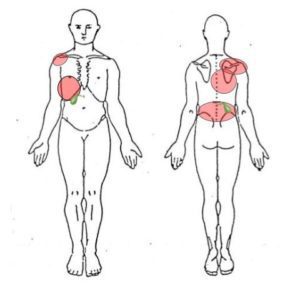
As you can see in the picture above, the gall bladder sometimes can cause pain in the lower right rib cage which is right where the gall bladder is. However, a lot of times, it is known to refer pain to the top in the back of the right shoulder, and less commonly the low back.
There are a couple of clues that you can look for to see if your pain in these areas might be coming from your gall bladder. The best clue is if you notice this pain more after you eat, especially after you eat things that are high in fat content, as this is when the gall bladder goes to work to help digest the fat. The other clue you can look for is in your stool. When the gallbladder is not functioning properly, the food that we eat will not be properly digested and absorbed, and it will come out in your stool. If you notice after you go to the bathroom that your stool is either floating on the surface of the water or sticks to the side of the bowl ,this can indicate that your body is not properly digesting fat and that the gall bladder is in trouble. These clues would tip you off that you need to see your primary care physician instead of a physical therapist or a chiropractor.
The final most common internal-organ referred pain that I see in my clinic is from the stomach and intestines. Oftentimes, our GI system doesn't present with very obvious symptoms when it's under stress. Therefore, many times the first symptoms that a patient notices is the pain referral.
As you can see in the picture above, the stomach and intestines can refer pain to many different areas. The most common area that many people already understand is that if they feel pain in their abdomen, they most likely have something going on in their stomach or intestines.
What I see a lot in my clinic is pain in the low back being caused by the stomach or intestines. This can actually happen for multiple reasons. Sometimes the actual structures in the stomach or intestines can refer pain to the back, but another common thing that happens is when your stomach or intestines are irritated, they will actually send signals to the brain to decrease the activation in your core muscles so that the muscles do not press hard against the internal organs. This reduction in core muscle activity can also lead to low back pain.
*Note: If you are suffering from low back pain, one of the best tips that I give people to determine whether this might be coming from the stomach or intestines is simply to pay attention to the sensations in their abdomen. You should not feel your stomach and intestines during normal digestion.
Sadly, in America, many of our diets are very poor and we eat lots of inflammatory foods. So it might be very common for you to feel a burning or irritation after you eat - but this is not normal. If you are experiencing low back pain, and you commonly notice that after you eat you feel like a burning sensation or a discomfort in your belly this is a big sign that your low back pain may be coming from the stomach or intestines. Your first stop should be your primary care physician.
Unlike some of the other organs mentioned above, referred pain in your stomach and intestines may require a trip to your chiropractor or physical therapist after you've seen your primary care doctor.
If your pain was coming from the inactivity in the core muscles that I mentioned earlier, you may require some core activation exercises to help return your body to normal and decrease your low back pain.
So there you have it. Our body can be very tricky! And understanding referred pain is the best way to shorten the amount of time it takes you to get better. Like I was saying above, if you're having chest pain and left arm pain and your doctor wastes time treating your left arm first, it's going to take you longer to get better. So make sure you see a doctor who is knowledgeable on referred pain.
If you're in the Tulsa area and are experiencing pain that you think might be referred pain, give us a call at 918-300-4084. Dr. John Keefe can do a thorough exam and let you know if his care would be right for you or if you should go see your primary care doctor.

Well - Halloween is fast approaching! As I was thinking about trick-or-treating, it made me think about the tricks that our body can play on us. So, for the month of October, I'm going to be covering the different ways that our body can trick us.
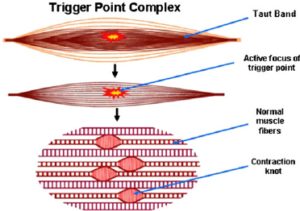
This week we're going to be talking about trigger points. You may have never heard of trigger points before, but you probably have felt them! When our muscles contract, the entire muscle does not contract all at once. If you start with your elbow straight and slowly bend your elbow, your bicep is one of the main muscles that does this action.
However, when you start to bend your elbow, the entire bicep muscle does not contract all at once. At first, the part of the bicep that's closest to your elbow is the only part that contracts, then slowly the middle portion of the bicep will contract, and then when your fist is up next to your shoulder, the upper portion of the bicep will be contracting.
This is how our muscles are supposed to work: Different sections contract depending on what our body is doing at that time - and then they relax when we stop moving that body part. At least that's how it's supposed to work. Sometimes little sections of our muscles will stay contracted even after we've stopped using that muscle. This tiny little section of muscle that remains in a contracted state is usually kind of hard to the touch. If you've ever felt a knot in a muscle, you're feeling a trigger point.
In this blog, I'm going to mention the different types of trigger points, trigger point pain referrals, and the three most common trigger point referrals I see in my patients that try to trick us about where the pain actually is.
There are two types of trigger points:
1) Active trigger points
2) Latent trigger points
If you're walking around and you feel a painful area in a muscle, that is an active trigger point. That means that it's painful at rest. But if you've ever had a massage, and when the massage therapist starts pressing on an area, you find that it's super tender and very painful, but it wasn't painful until they touched it, that is what's called a latent trigger point.
Trigger points are known to produce what is called referred pain. If you have ever heard of the symptoms of a heart attack, specifically the pain down the left arm, this is another example of referred pain. Referred pain is when one specific structure is irritated, but we actually feel the pain in other areas.
This can be extremely confusing, but it's very important to know if your pain is referred or not. Imagine if you went to the hospital with chest pain and left arm pain, and the nurses just started treating your left arm. You probably wouldn't have a very good outcome.
This is why it's important that your doctor is familiar with the concept of referred pain.
Otherwise valuable treatment time may be wasted on areas that are not actually irritated, but are just the location of referred pain.
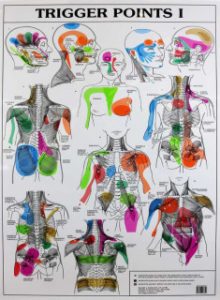
The woman who first discovered trigger points created maps of trigger point referral patterns. These maps showed the areas where referred pain is felt for all the different trigger points in all of the muscles of the body.
The three most common trigger point referrals that I see in my practice are:
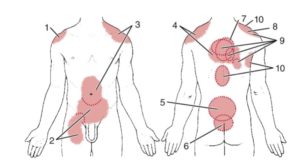
The gluteus medius muscles are located on the side of both hips. Trigger points in these muscles can send pain down the side and back of the thigh all the way to the back of the knee. Some doctors have called these trigger point referrals pseudo sciatica. Many people with trigger points in these muscles will actually think that they're having sciatica pain/issues, but really, it's just a trigger point.
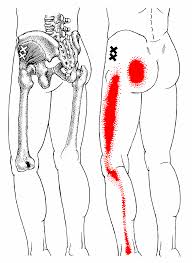
Above you will see the trigger point referral map for the gluteus medius. It can cause pain around the low back or SI joint and all the way down the thigh to the knee. If you are having pain in these areas, I recommend you get assessed by a doctor who's familiar with trigger points.
__________________________
The infraspinatus muscle is on the back of the shoulder. However, the trigger point referral actually wraps around to the front of the shoulder. Sadly, I have seen patients who had surgery on the front of their shoulder - and their pain didn't change at all. It was only after treatment to the infraspinatus on the back of the shoulder that their pain went away.
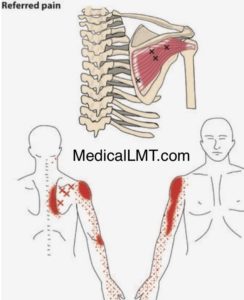
Above you'll see the trigger point referral map for the infraspinatus. It can cause pain along the inner shoulder blade area, the front of the shoulder, and down the bicep. If you've had pain in these areas and maybe even have had some treatment with no help, make sure to see a doctor who's familiar with trigger points.
_________________________
And finally, there is the thoracic erector spinae. The erector spinae muscles are the muscles that run up the spine very close to the bones of the spine. These are the muscles that help us stand up tall. In the thoracic region or mid-back, trigger points in these muscles can actually refer pain to the low back and tailbone. I will often see patients who complain of low back pain and have had lots of adjustments to the low back and pelvis with no improvement. Once we treat the erector spinae, their pain goes away.
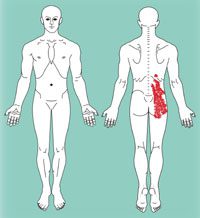
Above, you can see the trigger point referral map for the thoracic erector spinae. Interestingly, you can see that the pain referral map is almost completely in the low back. Meaning: You might not have any pain in your mid back, but that's actually where your problem is. These muscles can refer pain down to your low back tailbone and even the back of your hip. If this is a problem area for you - again - please make sure to see a doctor who's familiar with trigger points.
So there you have it, our body can really try to throw us for a loop. This is why it's always good, when you're in pain, to get a proper evaluation by a doctor who will look at all areas of the body and not just where you're hurting. This is something we do with every patient here at Movement Laboratory. If you're hurting and you suspect that you might have some referred pain going on or any other type of pain, give us a call at 918-300-4084 and we'll help you get out of pain fast!
Tune in next week when I'll discuss how some of our internal organs can cause pain all across our body!

This week I did a vlog continuing in the theme of foot and ankle stability. To truly have a stable foot and ankle you must have a stable hip. The one exercise that I think gives you the most bang for your buck for hip stability is called The Hip Airplane. In this vlog, go over all the different ways to regress and progress this exercise to match your current skill level. Make sure to check it out!
Foot Mobilization Vlog
This blog is in video format. In the video I go over three important mobilizations of the foot. In my previous blog I discussed the importance of stability of the foot and ankle. You cannot have proper stability in your feet and ankles unless you have proper Mobility as well. If you are lacking stability in your ankles try these foot mobilizations and see if your stability improves.

I've gotten a lot of feedback and questions about the feet in the last few weeks after I published my blogs on bunions. This week I wanted to talk about why our feet are so important for our overall health and wellness.
Our feet are literally our foundation.
They are the first thing that contacts the floor once we stand up and become weight-bearing. In addition to housing and maintaining the function of the muscles and joints that exist in our feet, there are also lots of nerves in our feet. Those nerves carry information to our brain and spinal cord that informs our brains about the structures of the environment around us.
If we are walking uphill, the nerves in the feet sense the stretch in the bottom of the feet from the hill and they begin to turn on the muscles that we use to raise our leg as we walk up the hill. If we are on uneven terrain, the nerves in the feet send messages to the brain and spinal cord that activate the stabilizing muscles in our hips that help to support us on uneven surfaces.
This is part of what makes the feet so important. As they encounter the ground around us, our feet send messages that help the rest of our body prepare for the environment that we are in. This is one of the reasons for the minimalist and barefoot trend emerging over the last 5 to 10 years. Much of our common footwear these days does not allow our feet to flex and bend and splay with the changes in our terrain. That limits the information coming in from the feet and makes our ankle, hip, and core muscles less able to anticipate the needs of the body.
Tightness in the feet and ankles can also limit this information. That is why foot and ankle mobility is so important. If your foot and ankle cannot bend and twist and splay, then those messages never get to the brain and spinal cord.
So this means there are two needs that our foot and ankle have to properly get our body ready to move.
In this blog, I will discuss how to make sure your foot and ankle get good exposure to the environment.
In my next blog, I will be going over how to make sure your foot and ankle have proper mobility.
The best way to make sure that your foot is able to sense the ground and the environment around you is to make sure that your footwear allows this to occur. This is why I recommend minimalist shoes for most feet.
When Minimalist shoes first came out, cushioning was thought to be bad, no matter what. And in my opinion, this is what caused many people to dislike minimalist shoes. Let's face it: If you are a marathon runner -- you're going to need some cushion. Thankfully, now minimalist shoes come with a wide range of features.
My recommendations for good Minimalist shoes for everyday use are the New Balance Minimus line, the Merrell vapor gloves, and splay shoes. These are really good shoes for going to work, working out, or walking or hiking. The links to find these shoes are below.
If you're looking for good Minimalist shoes for endurance sports like running, trail running, or long distance walking, I recommend Altra shoes and Topos. These are great foot-shaped shoes with no build-up in the heel and with good cushioning. The links to these shoes are below.
These shoes are a great first step to getting the most out of your foundation.
Additionally - and actually very importantly: I also recommend just walking barefoot in the grass as often as you can. Wake those feet up! Your body will thank you!
And remember, you can always check with me here at Movement Laboratory about any of your foot questions ---we're here at 918.300.4084 or dr.john@movlabtulsa.com.
Be sure to watch for my next blog about ensuring MOBILITY of your feet. It's a critical issue - and there are things you can do to increase your ability to move well on your feet!

Last week I went over the main things you need to know about bunions and how they affect you. This week we're going to cover what you can do to stop a bunion's progression or even reverse it!
So what does a strong foot look like? Well it's not what you think. We don't really need our feet to be especially strong - what we need is just for them to be active at the right times. Many people who have flat feet or bunions don't actually have weak foot muscles. It's more likely that they have weak hip and ankle muscles which then don't allow the foot muscles to activate like they should.
In order to have good strong feet, we have to be strong in other areas of the body as well. In this blog, I'm going to cover how to strengthen the feet, the ankles, and the hips. If you are strong in these three areas, that will stop the progression of bunions and sometimes even reverse them.
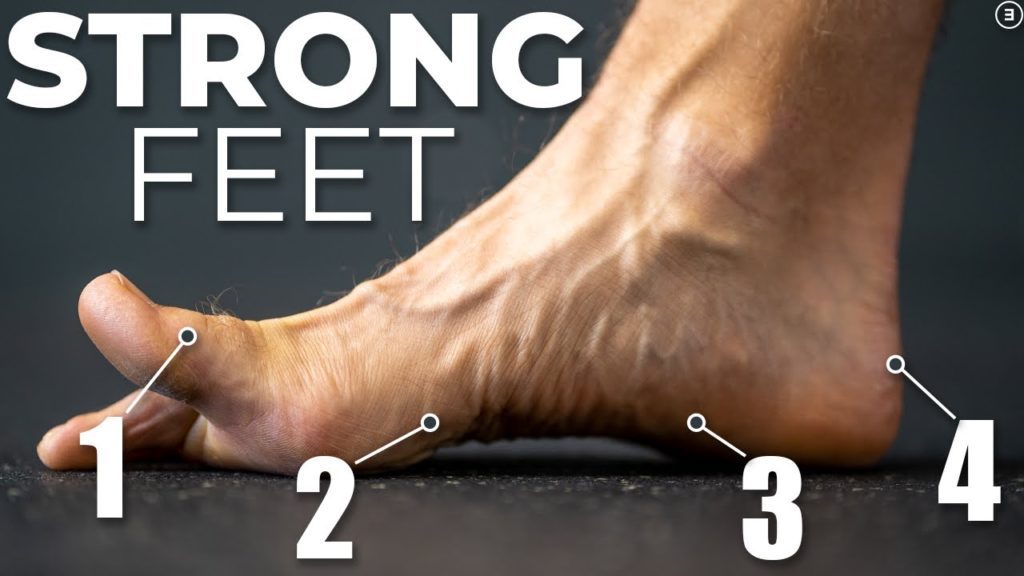
In order to strengthen the feet, we must first understand a little bit about how the foot works. The foot is constructed like a tripod. The three points of the tripod are:
A strong foot will keep these three points in contact with the ground as often as possible.
Our foot goes through a lot of different movements as we walk, climb, run and jump. The foot is meant to pronate, supinate, and be neutral and all the points in between. The issues that we have that lead to bunions tend to make our feet hang out most of the time in pronation. So in order to strengthen the foot, we need to strengthen the muscles that keep us either in neutral or supination.
The best exercise to help this is what's called the short foot exercise. When our foot pronates, it lengthens and becomes more wide. The short foot exercise helps to activate the muscles that do the opposite action. The video below shows how to do the exercise. I recommend doing just this exercise alone for two weeks. Usually doing about two to three sets of 10 at a time.
Once you feel confident doing this exercise, then you can start applying it to a lot of different situations.
Doing this will help to transition the short foot from being just an exercise that you do to something you can be practicing during your day in real world situations.
The next exercise to help strengthen your feet is called the Vele lean. This exercise is shown in the video below and it really helps to strengthen the muscles of the feet. The short foot practice combined with this exercise is a great one-two punch for strong feet!
The foot does not work alone. The hips and the ankles help to support the motions of the foot. You could have the strongest feet in the world, but if you have weak hips and ankles, your foot will still get in bad positions.
The first exercise to help strengthen your ankles is called the tibialis posterior raise. The tibialis posterior muscle is one of the prime supinators of the foot. If your foot over-pronates or pronates too fast, it means the tibialis posterior is not strong enough to resist that. The exercise is shown in the video below. I recommend doing three sets of 10 everyday.
Once you've helped to strengthen your tibialis posterior, it's time to work on the stability of the ankle. In order to do that, you have to challenge the ankle in a lot of different directions. The best exercise to do this is called toe reaches. The video below demonstrates this exercise. The key here is that you'll be standing on one leg and reaching the other leg out in different directions. Be sure that you try to keep the foot that is on the ground as still as possible. It is going to move a little bit. but you don't want it to be wobbling all over the place.
As I mentioned above, if your hips are not strong, your feet are put at a disadvantage. Bunions develop from feet that remain in pronation for too long. The hip muscles that help to bring the foot out of pronation are the external rotators of the hip, primarily the gluteus, medius, maximus, and piriformis.
A great first exercise to start strengthening these muscles is called a glute bridge with abduction. The exercise is shown in the video below. I usually have people start with two sets of 10 and slowly work up to three sets of 12.
The next exercise is a great one because it can work on almost all of those muscles at once. It is called a lateral band walk. The video is shown below. Pay special attention to the placement of the band. By placing the band around the foot instead of the ankles like this exercise is normally done, it really works on those external rotators of the hip.
The final exercise really works on increasing control of the hip rotators. This exercise is called the hip airplane. When you start this exercise, you'll want to be close to a wall or a table that you can use for balance. After a couple of weeks doing the exercise, you need to start taking your hand off of whatever structure you're using for balance, and starting to try to balance on your own. Eventually you want to be able to do this exercise without using anything for balance.
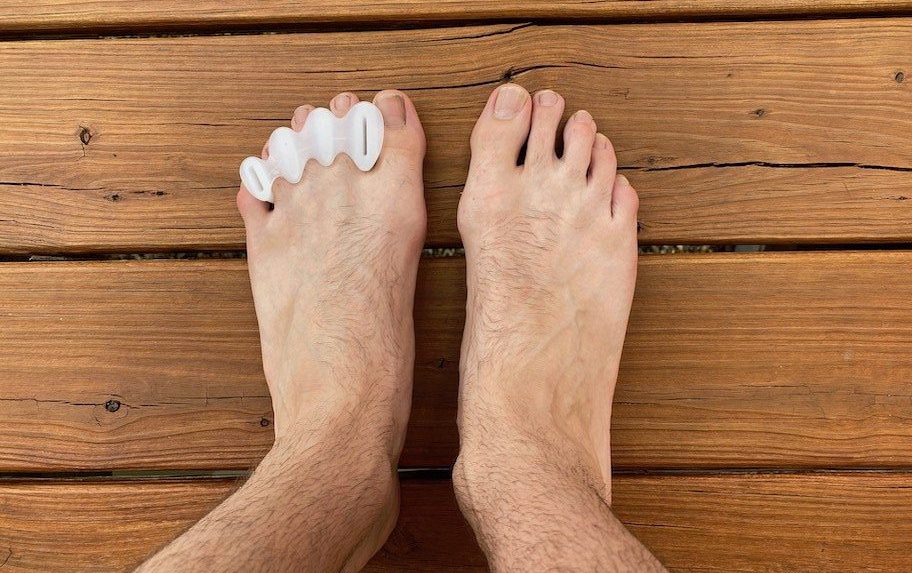
Special/Simple Device to Help Stop/Correct Bunions
One final recommendation for stopping bunions or reversing them is actually a device to wear on your feet. This device is called correct toes. This simple silicone piece can be worn at all times even with socks and helps to maintain the placement of the toes which can help the deformation of the bunion. I recommend this for all bunions! They can be purchased here: https://www.correcttoes.com/shop/correct-toes/correct-toes.html?gclid=CjwKCAjwrqqSBhBbEiwAlQeqGrrmlzau3uTeVCbstoyU37gGT-kNmsutB_DoQC7TX_qjHgJxF1TZVhoCHBgQAvD_BwE
_________________________________________________
So there you have it. If you have a bunion, or if you're wanting to make sure you don't develop a bunion, this program includes my recommendations to make sure you know what to do to help ensure those results! And if you are looking for more help with your feet, give us a call at Movement Laboratory at 918-300-4084 and schedule an appointment today. We help get people moving better and out of pain fast!


We've all seen them - some of you may be starting to notice them on yourselves, some of you may be dealing with them for years. That's right - today, we're talking about bunions!
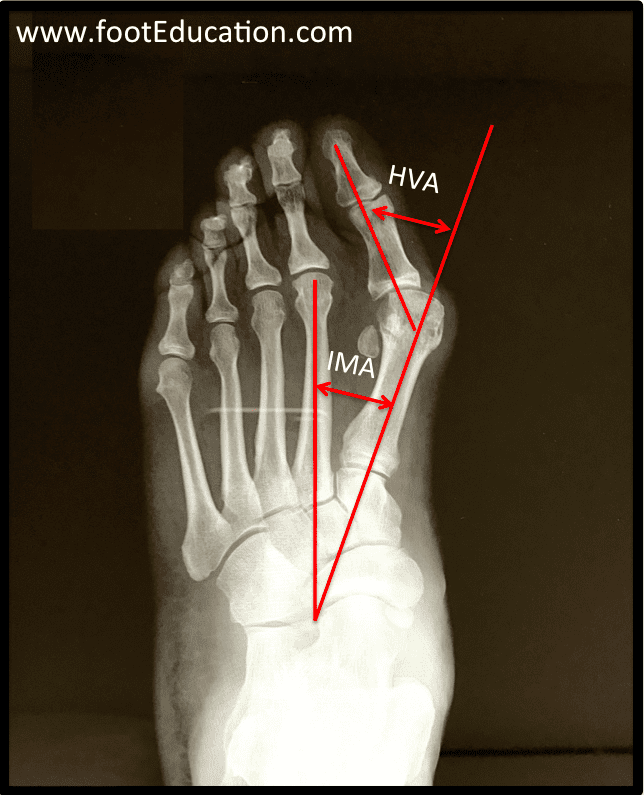
Oh bunions! According to some, one of the ugliest deformities that can happen to our feet. In today's blog, I'm going to talk about what bunions are, and why they happen. Next week, I'll address ideas for things we can do to prevent bunions and what we can do to help improve a bunion that's already in progress.
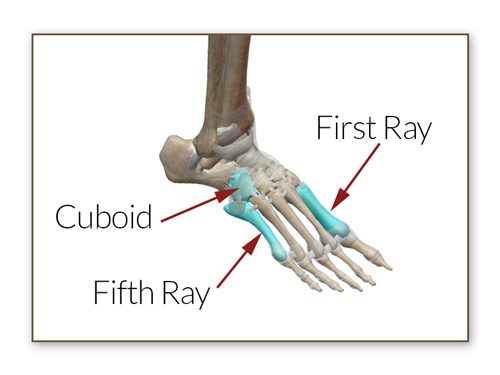
In order to talk about bunions, we're going to have to talk about some anatomy first. The central driver of bunions is a bone in our foot called the first ray or first metatarsal. This is the long bone that goes from your ankle to your big toe.
The first ray is extremely important in our everyday movements. It bears a ton of weight whenever we push off of our feet as we're stepping forward in a process called toe-off. The first ray's movement is a big part of pronation and supination of the foot which is what allows our foot to absorb impact as we walk, run, jump, and climb.
When you step forward while walking, your heel is the first thing that strikes the ground. When your heel strikes the ground, your first ray is pointed downwards. As the foot rolls forward from the heel and weight gets transferred into the rest of the foot, your foot transitions from supination to pronation. This causes the weight to roll up the outside of the foot across the balls of the foot, to the ball of the big toe, then eventually the weight rolls off the big toe as we step forward.
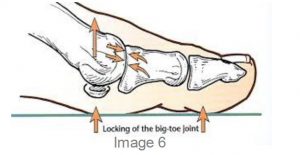
During this process, the first ray starts out pointed downwards or flexed, and slowly starts to move upwards as our foot pronates and flattens out while our foot gets ready to toe off as we step forward. This is part of the process of pronation. Many people are under the impression that pronation is bad. However this couldn't be further from the truth. If our foot could not pronate, we would not be able to walk or run.
Pronation is not a bad thing - overpronation or extremely rapid pronation is what is bad for our feet. The foot and ankle are supposed to slowly pronate as the weight shifts from the heel to the big toe. But this process is supposed to be slow and gradual. Weakness in our foot and ankle muscles will sometimes allow this process to happen much faster than it's supposed to and that's where problems occur with pronation.
When our heel lands as we step forward, our foot is in a supinated position. When the foot is supinated, it is relatively skinny. As the heel strikes and our weight shifts forward into the balls of the feet, our foot flattens out and becomes wider. As this happens, the first ray moves from being at a downward angle upwards and becomes more of a flat angle; it also spreads away from the other bones of the foot as the foot widens.
One part of our anatomy that is very important for this process is a muscle called the adductor hallucis. As the first ray widens and spreads out, and moves towards the other foot, the adductor hallucis helps to slow the inward movement of the first ray, helping pull it back into position as we toe off and the foot moves back towards supination as it steps forward.
Bunions develop when the muscles of the foot and ankle cannot slow the rate of pronation and the foot flattens out too much, making it unable to return to its normal width at the appropriate time in the step process. When the foot remains in this widened position for too long, the adductor hallucis begins to weaken and lengthen. This allows the first ray to move inwards. Due to the way the other foot muscles are attached to the big toe, the big toe will stay in its previous position. So as the first ray moves inwards with the big toe staying where it is, the foot develops the angular deformity known as the bunion.
These are the basic biomechanical, internal body issues that can lead to bunion formation. However, there are also other external factors that can worsen this process. One of the most common external factors that make the formation of bunions more likely to occur is our footwear.
We have decided as a culture that footwear is more attractive when it's not actually shaped like our feet.
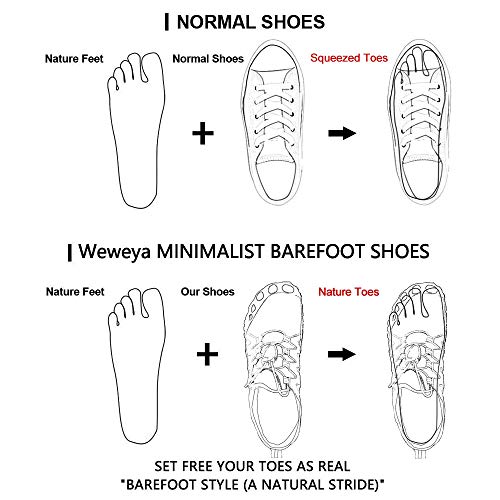
Humans are weird! We have decided as a culture that footwear is more attractive when it's not actually shaped like our feet. Most shoes get skinnier towards the toe. But that's not how our feet are shaped. This skinniness in the toe box leads to the 1st and 2nd toes, and the 4th and 5th toes being pushed in towards the third toe.
So basically, a high percentage of our footwear encourages bunion formation. If you add together all of the internal biomechanical feet factors and the external issue of inappropriate footwear, our sedentary lifestyles that lead to weakness in our hip and ankle muscles, our lack of time spent barefoot in order to strengthen the muscles of our feet, and the general shape of our footwear, all of this is the perfect storm for bunion formation.
_______________________________________________
Ah, Bunions!
So there you have it. That is a simple explanation of what a bunion is and how it forms. In my next blog. I'll discuss what you can do to try to prevent bunions, along with some ways you can choose to try to stop the progression and even reverse the progression if you're already dealing with a bunion.
So make sure to stay tuned for next week!
_______________________________________________
And as always, if you're dealing with bunions or other foot-related pain, or pain anywhere else in your body, we here at Movement Laboratory are here to help. You don't have to just deal with pain and let it limit your life. Call us today at 918-300-4084, get an appointment scheduled, and let us help you quickly get out of pain and back to doing what you love!
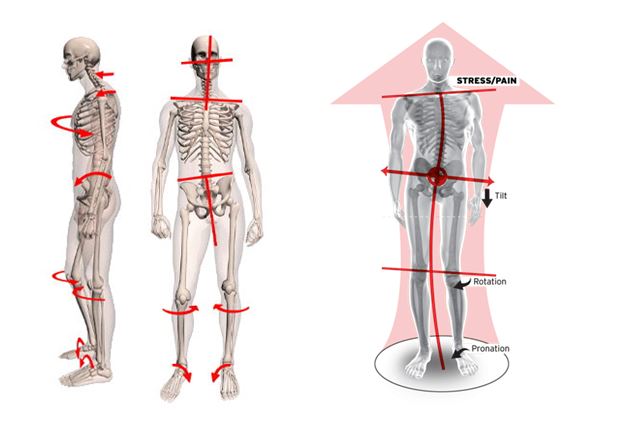
We've all heard that old song as kids: "The foot bone's connected to the ankle bone." But what we may not know is that that song is actually very true. Our feet can affect our entire body. A great example of this is a research study that found that hyper-pronation of the foot can lead to TMJ pain in the jaw.
In this blog, I'm going to cover three of the main conditions I find on a regular basis when my patients have pain in other areas of the body - but it's actually being caused by issues with their feet and ankles.
At first glance, the knee appears to be a pretty simple joint; it looks like it's a simple hinge. But looks can be deceiving. The knee not only bends like a hinge, but it also rotates inward and outward and can translate forward and backwards.
There's a saying in the healthcare world, "The knee is a slave to the hip and ankle". A great way to see this for yourself is to stand up and try to move your knee without moving your hips or ankles. It's impossible!

If you have an unstable foot with either too much pronation or supination, this will put your knee in a vulnerable position. An over-pronated foot will cause increased stress on your inner knee and an over- supinated foot will cause increased stress on the outer knee.
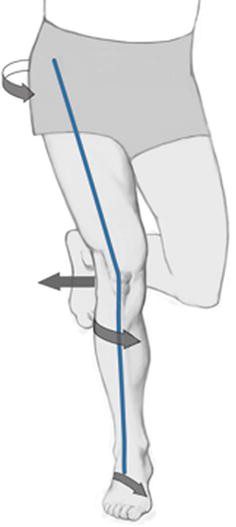
Stiffness in your foot and ankle leads to pain in the front of the knee and around the kneecap. This is one of the most common types of knee pain that I see in my practice. Pain around the kneecap is often accompanied with both stiffness in your ankle and instability in the foot, so that condition needs a proper assessment by a healthcare practitioner to facilitate the quickest healing.
The hips can also be impacted by issues in the feet. Instability in the foot and ankle can lead to pain on the outer hip and posterior hip, and can also lead to pain in the groin. Stiffness in the ankle most commonly can lead to pain in the front of the hip.
When the foot over-pronates, it causes the knee to "cave in" - this leads to increased stress in the outer hip muscles (the gluteus medius) and increased stress in the back of the hip in the piriformis muscle.
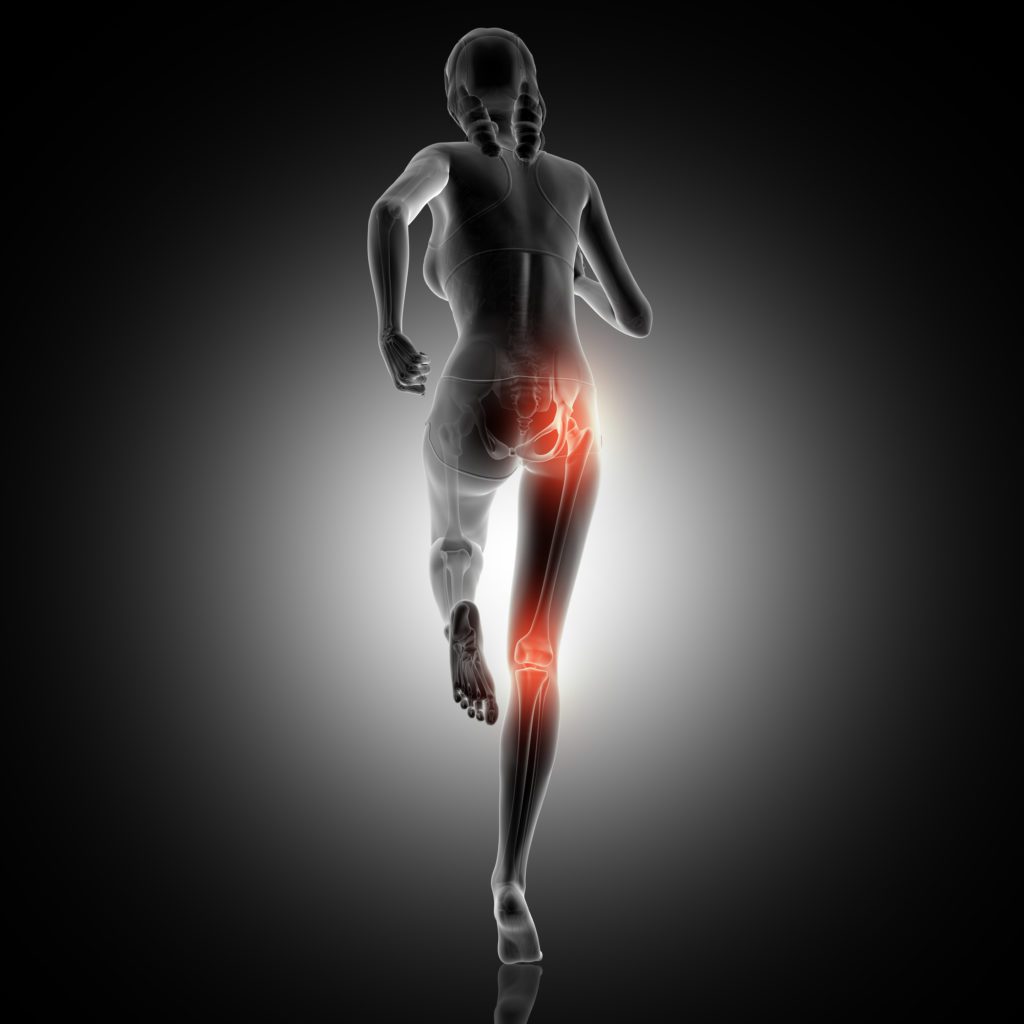
When we have a stiff ankle, it causes a change in the final stage of the gait cycle called "toe-off". When we step forward, our weight is supposed to shift forward while our ankle flexes; this allows our leg to push us forward. When the ankle is stiff, that can lead to excess force needed in our hip in order to step forward. That situation will cause pain in the anterior or posterior hip.
The feet and ankles can also be a primary component of low back pain. Anytime we utilize squatting motions, such as sitting in a chair, squatting down to pick something up, or jumping, our ankles need to bend.

When our ankles are stiff, in order to get our hips lowered such as to allow us to sit in a chair, we have to bend our back more than is necessary to accomplish that task. So stiffness in the ankles will cause increased stress and pain in the low back.
Instability in the feet and ankles will also cause a rotation in our pelvis. When our pelvis is not able to be in a neutral position for long periods of time, this causes increased stress in the muscles and ligaments of the low back. In this case, this causes under-pronation or over-supination, either of which can also be a contributor to low back pain.
The most important thing to understand in considering how instability, over-pronation, or over-supination, and other feet/ankle conditions can affect areas like the knee, hips, low back - or even the jaw - is that we may only feel pain and discomfort in the other areas. This means we may not realize that our feet and ankles are the problem because we don't feel any pain there.
This is why it's important to see a healthcare practitioner who evaluates the entire body - not just the area that is hurting. At Movement Laboratory, every new patient gets a full-body movement assessment; no matter if the complaint they're coming in for is neck pain, knee pain, or wrist pain, or another area. It's critical to check how each area's mobility range and level affects the rest of the body.
A proper comprehensive evaluation will save a ton of time in recovery. So - if you're dealing with any of the issues listed in this blog, come see us at Movement Laboratory to get feeling better as fast as possible! Just give us a call at 918-300-4084 or you can even book online at movlab.janeapp.com.